You had a headache and you purchased over-the-counter paracetamol. You took two tablets of the medicine and swallowed them with water (or some other juice). After a while, presto! The headache was gone! ….. or persisted! Either way, oral drug delivery is easy, painless, and quite cost effective compared with other forms of drug deliveries like virginal/anal, buccal mucosa (lining of the cheek), or subcutaneous injection.
Your gastrointestinal tract (GI) is the passageway of the digestive system that leads from the mouth to the anus, and includes the oesophagus, salivary glands, liver, gallbladder, pancreas, stomach, and intestines. There are all sorts of activities happening along the GI: microorganisms catabolising and metabolising, enzymes and mucous being secreted, acids produced, excretory pumps, etc. A good example of how messed up your GI is, is to look at the byproduct of the food you consumed about 48 hours ago. That bowl of good-looking and sweet-smelling fried rice, chicken, cow meat and plantain you just ate, in the next 48 hours or so, the byproduct (your poo) will come out looking and smelling something quite different from the food you ate.
Join our WhatsApp ChannelMedicines taken orally will need to jump through a lot of hurdles in the body before reaching the areas they are needed. An oral drug must overcome the acidic environment of the stomach, be able to resist degradation by enzymes along the GI, be able to dissolve in the gastrointestinal fluid, evade being pumped out, be able to get absorbed and transported easily in the blood, be able to penetrate the viscous mucous barrier in the intestine, and must be in enough concentration at the required site to be effective.
Few drugs possess all the above attributes; therefore, alternative routes of administration are used for effective delivery of some drugs. For example, insulin is required by diabetic people, but when given orally, the availability level required for it to be effective (i.e. bioavailability level) is reduced to less than 1%, hence it is more effective when given by subcutaneous injections. But many people who are afraid of needles tend to shy away from injections. Oral drug delivery suffers from the harsh degradative environment of the gastrointestinal tract and poor absorption of these drugs. Therefore, an effective drug delivery method to overcome the problems of distribution in the body, absorption in blood, metabolism, and elimination, are important so that patients can receive the necessary medical therapy for their ailments.
There are many efficient drug delivery technologies developed in the recent times, for example, nanoparticles (which could cross the blood–brain barrier, BBB), ultrasonic vibrations, micro-stirring pills and liposomes that are designed to penetrate the mucous layer of the intestine called the intestinal epithelium. The only problems with these technologies are that they are specific for individual drugs and therefore require optimisation for each drug. Also, due to the nature of their design, they are not always convenient for everyday clinical application.
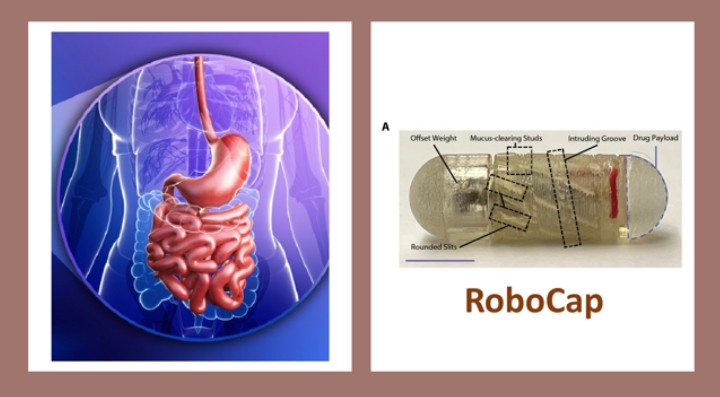
Scientist working at the Massachusetts Institute of Technology (MIT), USA, have developed a robotic capsule they called “RoboCap”. This robotic capsule, which is orally ingestible, could clear away the mucous lining the intestinal tract and deliver its cargo drug to the required area of the small intestine. This makes it possible for rapid absorption of the drug into the target area.
Caution: if you are not technically minded, you may wish to skip the next two paragraphs:
Writing in the October 2022 issue of Robotic Science, the researchers described the RoboCap as equivalent in size as a large multivitamin pill. The RoboCap has a cargo-hold where the drug it is meant to deliver is stored. And to prevent the device damaging delicate tissues or the patient experiencing some discomfort in swallowing the device, it is covered in gelatinous coating. When the patient swallows the RoboCap, it travels to the stomach where the gastric acid of the stomach degrades the gelatinous coating. The RoboCap swims to the small intestine and a change in pH dissolves a pH-sensitive membrane contained in the Robocap triggering the closure of an electrical circuit.
The closure of this electrical circuit activates an offset weight connected to a motor, which generates the centripetal force needed for the RoboCap to begin to spin around. As the RoboCap rotates, its helical surface and studded texture interact with the plicae (large circular folds of tissue), villi (microscopic finger-like protrusions) and mucous on the surface of the intestine, clearing away the mucus layer. With each rotation of the RoboCap, the drug payload is then gradually released in the cleared area. Thus, the drug is deposited directly onto the intestinal surface. The RoboCap is active for approximately 35 minutes before it is passed outside the body during defecation.
The proof of the pudding is in the eating. Delivery of two drugs using the RoboCap was conducted by the scientists. The two drugs used in this trial were insulin and the antibiotic, vancomycin. RoboCaps or sham pills carrying 100 mg of vancomycin were placed into each isolated section of the small intestine of an anaesthetised pig. A second delivery test was conducted with RoboCaps carrying 100 units of insulin and as controls, sprays of insulin in the small intestine were used.
The data showed that RoboCap delivery of vancomycin resulted in the permeability of the drug into the tissues by more than 20 times compared with the control. Furthermore, there was a significant increase in the concentration of vancomycin in the surrounding veins, which was not seen in the control samples. Delivery of insulin through the RoboCap significantly increased insulin levels in the blood and a sharp decrease in glucose levels was observed compared with the controls.
The RoboCap is designed with practical considerations. The position of the drug payload, which is at one end of the capsule, allows for a drug of choice to be loaded by the pharmacist. Also, the pH sensitive nature of the RoboCap can be exploited to target other areas of the GI tract simply by changing the properties of the dissolved membrane to the required pH of the targeted area.
The RoboCap safety issues were addressed. Oral delivery of the robotic capsule was monitored by endoscopy. An endoscopy is a long flexible tube inserted down the throat and into the oesophagus. At the end of this tube is a tiny camera, which makes it possible to examine the oesophagus, stomach, and the duodenum (i.e. the beginning of the small intestine). Endoscopic examination before and after oral delivery of the RoboCap shows “No erosion of the mucosa, inflammation, infection, or haematological complications were sustained.”
However, there are a few concerns and room for improvement in the RoboCap application. The role of the mucous barrier lining the GI epithelium is to protect against pathogens. Therefore, excessive mucous clearing might result in risk of infection. But this scenario is prevented by the frequent turnover and constant mucous production by goblet cells in the epithelium.
The robotic capsule is not suitable for use in patients undergoing MRI (magnetic resonance imaging) because of the presence of a metal within the capsule. In such a situation, PillCam can be used instead of MRI. PillCam is a device the size of a tablet, which contains a small camera and when swallowed takes pictures of the inside of a body.
Given the leaps and bounds of technological advances, it is envisaged that a wireless version of the robotic capsule could be developed in future. This would remove the rigid electronics inside the current RoboCap model.
Effective drug delivery techniques, such as the RoboCap, are certainly welcome prospects, especially in delivering drugs to those affected areas of the body, which due to the delicate natures of the diseases e.g. cancers, are inaccessible or poorly covered by conventional drug delivery systems.


![Relishing Ugba [Oil Bean] Delicacy](https://www.primebusiness.africa/wp-content/uploads/2025/06/Ugba-delicacy-720x480.jpg)













Follow Us