Type 1 diabetes is a condition that occurs when the body does not produce insulin to control blood sugar levels.
The condition is characterised by the body’s immune system attacking and destroying the insulin-producing cells found in the pancreas. Those diagnosed with Type 1 diabetes need lifelong insulin therapy to manage their blood sugar levels.
Join our WhatsApp ChannelThe risk of hyperglycaemia, whereby the level of sugar in the blood gets too high, is common in persons diagnosed with Type 1 diabetes. Hyperglycemia can damage the eyes, nerves, heart, and kidneys, and can lead to stroke. Increased frequency of passing urine, feeling thirsty, tiredness, and fruity breath are symptoms of hyperglycaemia.
Conversely, hypoglycaemia is when the blood sugar levels are low. This can lead to shakiness, confusion, and accidents, especially if the person is driving or operating heavy machinery. In severe cases of hypoglycaemia, seizures, coma, and even death can occur. Among people with Type 1 diabetes, more than a quarter do not have any warning signs that their blood sugar levels are falling dangerously low. Patients with this type of condition are said to have Type 1 diabetes with impaired hypoglycaemic awareness and severe hypoglycaemia.
A new stem cell-derived therapy called, zimislecel, might just be the wonder weapon to relieve people with Type 1 diabetes of their suffering and the inconvenience of daily injections of insulin. Zimislecel is an experimental donor-derived stem cell therapeutic drug produced by Vertex Pharmaceuticals, Boston, USA. As reported in the June 2025 edition of the New England Journal of Medicine by Reichman and coworkers, lab-grown pancreatic beta cells were implanted into the liver (rather than in the pancreas), where they start to produce insulin to regulate blood sugar levels (apologies for not describing the technology in detail, it is Vertex Pharmaceuticals’ trade secret).
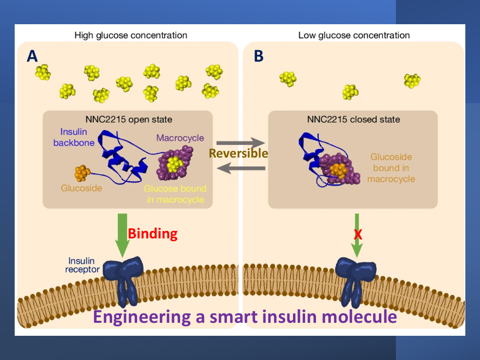
READ ALSO: A Smart Insulin Switch For Regulation Of Diabetes
Zimislecel recently underwent a phase 1-2 clinical trial with just 14 participants drawn from patients susceptible to Type 1 diabetes impaired hypoglycaemic awareness and severe hypoglycaemia. The drug was delivered to participants as a single infusion into the hepatic portal vein. Participants also received immunosuppressive medication to avoid an immune reaction to the foreign transplanted cells.
All the 14 participants showed evidence of islet engraftment and function, i.e., the infused pancreatic islet cells were able to replace non-functioning indigenous cells and produce insulin in response to glucose levels. Participants who received a full dose of the drug (0.8×10⁹ cells) were free of any adverse hypoglycaemic events. Within a year of receiving a single full dose of zimislecel, 10 participants were fully insulin-independent. In other words, their liver was able to produce enough insulin to regulate blood sugar levels without any recourse to exogenous insulin.
READ ALSO: Diabetes Patients Groan As Monthly Medication Rises To N150,000
However, the clinical trial was not without problems. Three participants developed neutropenia (ie abnormally low level of neutrophils. Neutrophils are a type of white blood cell that the body needs to fight infection). The neutropenia was no doubt caused by the accompanying immunosuppressive therapy given to participants.
Two deaths were also, reported during the therapy. One death occurred in phase 2 of the clinical trial and was caused by cryptococcal meningitis due to sinus surgery and steroid treatment unrelated to the study. The other death, which occurred in phase 1 of the clinical trial was attributed to severe dementia as a result of progression of preexisting neurocognitive decline.
Cryptococcal meningitis is a fatal fungal infection of the brain and its surrounding meninges (it is called cryptococcal pneumonia if the lungs are infected). Cryptococcosis occurs in both healthy and immunocompromised individuals and is caused by inhaling fungal spores from the environment. But immunocompromised persons, especially those taking immunosuppressant therapy are particularly at risk from the disease. Therefore, it could be speculated that a weakened immune system resulting from a combination of immunosuppressive therapy and a high-dose steroids regimen, might be a contributory factor for the death by making the patient susceptible to infection.
The trial results are quite encouraging but it meant that patients receiving this type of treatment would be on lifelong immunosuppressive medication to prevent the destruction or rejection of the engineered islet cells by the body’s immune system. This means that patients are predisposed to infections because the levels of their infection-fighting white blood cells (ie neutrophils) are compromised.
There is an issue worth bearing in mind. People with Type 1 diabetes may have been presented with a Hobson’s choice with the discovery of this stem cell therapy. In the absence of the more expensive and limited-donor pancreatic transplantation, it is either the patients have insulin-independence by undergoing zimislecel stem cell treatment and run the risk of compromised immune system or retain their natural immunity and continue with their daily injection of insulin but run the associated risks involved in episodes of Type 1 diabetes impaired hypoglycaemic awareness and severe hypoglycaemia.
READ ALSO: Anti-Obesity And Diabetes Drugs May Also Enhance Fertility
Additionally, the number of participants in the clinical trial is very low to predict with any degree of confidence that the same encouraging results would be obtained in a larger sample size. While the study implicitly demonstrates the ability of zimislecel to restore insulin production in cases of Type 1 diabetes, the phase 3 clinical trial should focus on expanding the sample size, which currently is aimed at recruiting 50 patients. The duration of the clinical trial should also be extended to allow for the effect of immunosuppressive therapy on patients to be empirically assessed.
This stem cell approach to treating Type 1 diabetes is revolutionary and gives hope to millions of people in the world currently living with the condition. The technology can be a source of unlimited supply of beta cells for transplantation unlike pancreatic transplantation, which is limited by the number of donors available. If the technology passes its phase 3 clinical trial and gets FDA approval, it should be a significant toolkit to the fight against Type 1 diabetes.