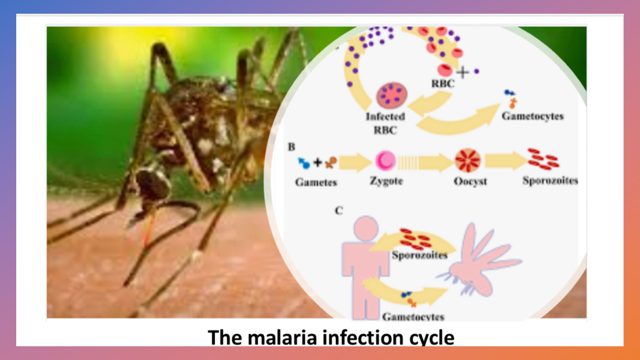
IN the treatment of malaria, multiple drugs are deployed. This is because malaria parasites are notorious for developing drug resistance. By deploying multiple drugs, it is more difficult for the parasites to develop resistance against the drug cocktail. In this regard, the gold standard for the treatment of malaria is artemisinin and its derivatives. A combination of the aforementioned with “partner” drugs is called Artemisinin Combination Therapies (ACTs).
In the mid-2000, reports started emerging of Plasmodium falciparum malaria parasites developing resistance to artemisinin and its derivatives. This resistance progressed to evasion also of some of the partner drugs in the ACTs by the parasites. But this drug resistance to ACTs was confined to Asia until recently when it has been confirmed that it has arrived in Africa.
Join our WhatsApp ChannelThe newly reported drug resistance to ACTs in Africa was independent of the Asian resistance, which is troubling for it means that with time the resistant malaria parasite strains might evolve into “super” resistant parasites. It is bad enough that about 90% of reported malaria death occur in Africa but to also add drug resistance into the mix will be a tragedy.
The study recently reported in the New England Journal of Medicine was conducted in Northern Uganda between 2017 and 2019. In the study, 240 people with malaria caused by P. falciparum were treated three times daily with intravenous artesunate, which is a very powerful artemisinin derivative. This was followed by a standard three-day course of ACTs pills.
People suffering from malaria normally clear half of the parasites in their system within two hours upon treatment with artesunate. But in the study, 14 participants were found to have taken more than five hours to clear half of the malaria parasites. Upon examination, the parasites in 13 of these 14 people had undergone mutations in a gene called the kelch13. Mutations in this gene are principally responsible for drug resistance by slowing down artemisinin activation due to reduced haemoglobin endocytosis.
The World Health Organisation has validated 10 kelch13 mutations in P. falciparum as molecular markers for artemisinin resistance and recognised extra 13 kelch13 mutations as associated markers. In the Ugandan study, 7 kelch13 mutations were detected in 38 out of the 240 subjects.
In another study conducted in 2018 and published in the August 2021 edition of Lancet Infectious Diseases, children from Rwanda suffering from malaria were given a three-day course of ACTs pills. It was discovered that some of the children still had malaria parasites in their system after completing this three-day course of treatment. Malaria parasites from these children were analysed and found to have had two kelch13 mutations, which were different from those seen in the Ugandan study.
The researchers in the Ugandan study attributed one of the causes of this resistance development to artemisinin and its partner drugs by the P. falciparum parasites, to the excessive use of injectable artesunate. This might have resulted in selective pressure for resistant P. falciparum parasites. But don’t hit the panic button yet, because ACTs still work albeit do require a longer time than normal. An alternative approach to malaria treatment specially adapted to sub-Saharan Africa and which still works normally is another ACTs combination of artemether (a derivative of artemisinin) and a partner drug called lumefantrine.
Nevertheless, nobody knows how widespread Africa this problem of malaria drug resistance is. But judging by the evidence presented in this study and the one conducted in Rwanda, the assumption is that the problem is widespread. Therefore, there is an urgent need to act quickly and find alternative drugs of choice different from ACTs to avoid a repetition of the death toll experienced in the late 20th Century when malaria parasites developed resistance to chloroquine. In this regard, the advent of malaria vaccines should also help in the fight against the disease.